IVD of Cardiovascular
🧪 CKB-2729H
Source: E.coli
Species: Human
Tag: His
Conjugation:
Protein Length:
🧪 APOA1-33H
Source: HEK293
Species: Human
Tag: Fc
Conjugation:
Protein Length: 1-267 a.a.

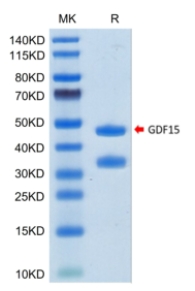
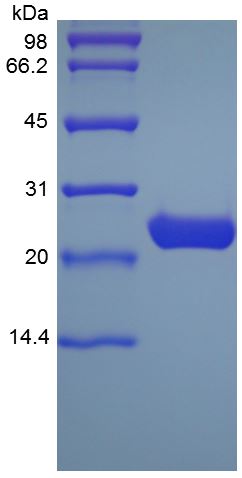
🧪 GDF15-204H
Source: HEK293
Species: Human
Tag: Fc
Conjugation:
Protein Length: Ala197-Ile308
🧪 IL1RL1-775H
Source: HEK293
Species: Human
Tag: Non
Conjugation:
Protein Length: 1-328 a.a.
🧪 REN-317H
Source: HEK293
Species: Human
Tag: His
Conjugation:
Protein Length: Met1-Arg406

🧪 APOA1-698H
Source: E.coli
Species: Human
Tag: Non
Conjugation:
Protein Length: 243
🧪 GDF15-337H
Source: CHO
Species: Human
Tag: Non
Conjugation:
Protein Length:

🧪 APOE-2630H
Source: S.frugiperda
Species: Human
Tag: Non
Conjugation:
Protein Length: 112-158 a.a.
🧪 Crp-3291M
Source: HEK293
Species: Mouse
Tag: His
Conjugation:
Protein Length: 1-225 a.a.
🧪 MB-2165W
Source: E.coli
Species: Sperm Whale
Tag: Non
Conjugation:
Protein Length:
🧪 IL1RL1-3991H
Source: HEK293
Species: Human
Tag: His
Conjugation:
Protein Length: Met1-Ser328
🧪 LGALS3-453H
Source: E.coli
Species: Human
Tag: GST
Conjugation:
Protein Length: 1 - 250 aa
🧪 PLA2G7-1145H
Source: HEK293
Species: Human
Tag: His
Conjugation:
Protein Length: Met1-Asn441

🧪 Crp-4095R
Source: HEK293
Species: Rat
Tag: His
Conjugation:
Protein Length: 1-230 a.a.
🧪 FABP3-6927H
Source: E.coli
Species: Human
Tag: Non
Conjugation:
Protein Length: Met1-Ala133
What is Cardiovascular Disease?
Cardiovascular disease is a term used to describe an assortment of diseases that affect the heart and blood vessels. It is usually caused by accumulation of fatty deposits in the arteries and increased risk of blood clots. It can also be associated with the destruction of arteries in the brain, heart, kidneys, and eyes.
The most common forms of cardiovascular disease are coronary artery disease, stroke, heart failure, arrhythmia, and heart valve issues. Poor diet, obesity, and smoking are the major lifestyle risk factors for cardiovascular disease. And so does genes and age.
An active lifestyle can help you stay away from cardiovascular disease. This means eating a well-balanced diet that contains a lot of fruits and vegetables, getting enough exercise, keeping your weight in check, and never smoking. Additionally, regular visits to your doctor can monitor and control risk factors such as high blood pressure, cholesterol, and diabetes.

What are the main types of cardiovascular disease?
Coronary Artery Disease (CAD): CAD is one of the most common cardiovascular diseases. It occurs when the coronary arteries that carry blood to the heart muscle narrow or become blocked by accumulation of cholesterol and fatty deposits (plaques). This can result in chest pain (angina), shortness of breath, or even heart attacks when the blood supply is severely limited or interrupted.
Heart Failure: Often misunderstood as the heart stopping, heart failure actually refers to a heart's inability to pump the blood the way it should. It may occur for various reasons, such as high blood pressure, damage to the heart muscle from a previous heart attack, or chronic conditions that weaken or stiffen the heart muscle.
Arrhythmias: These are irregular heartbeats that can be either too fast, too slow, or erratic. Arrhythmias come in many forms, and atrial fibrillation is one of the most prevalent. We need to control them because they influence the heart works.
Heart Valve Problems: Four valves of the heart open and close as gates that manage blood flow. Problems with valves – stenosis, regurgitation or prolapse – can disrupt this flow, putting extra strain on the heart and affecting its function.
Congenital Heart Disease: It includes various birth defects that cause changes in the structure and function of the heart. Some of these can be diagnosed at birth; others may take a lifetime to emerge.
Peripheral Artery Disease (PAD): This condition affects the blood vessels outside of the heart and brain. It usually means a narrowing of the arteries to your extremities (most often the legs), a stabbing or cramping sensation when you walk, and a general build-up of fat deposits in your arteries.
Aortic Disease: The body's largest artery, the aorta, can become damaged by aneurysms and other injuries. An aortic aneurysm is a bulge in the artery wall that, if ruptured, could be life-threatening.
Clinical Information
What does cardiovascular symptoms?
Chest Pain or Discomfort: More commonly, a feeling of pressure, tightness, swelling, or discomfort in the chest.
Shortness of Breath: This can be coupled with or without chest pain and might be a sign that the heart isn't pumping efficiently.
Pain, Numbness, Weakness, or Coldness: Can occur in the legs or arms if blood vessels in those regions of the body are clogged.
Pain in the Neck, Jaw, Throat, Upper Abdomen, or Back: These symptoms can accompany chest pain, particularly in women.
Fatigue: Having a high level of tiredness is a symptom of heart failure or other cardiovascular problems.
Swelling in the Legs, Ankles, or Feet: This can be a sign of heart failure or a problem with blood flow through the veins.
IVD methods used in cardiovascular diseases analysis
IVDs play a significant role in the diagnosis and treatment of cardiovascular conditions. IVD protocols usually consist of blood testing for the presence of markers for heart disease. These tests can include cholesterol profiles, cardiac biomarkers such as troponins (which go up after a heart attack), and genetic tests for risk factors for hereditary heart disease. These tests detect and treat cardiovascular disease early, influencing therapies and potentially leading to better outcomes.

What are the causes for cardiovascular disease?
Cardiovascular disease (CVD) can be caused by multiple causes, many of which have to do with lifestyle, genetics and other health conditions.
High Blood Pressure (Hypertension): Chronic high blood pressure can damage arteries, leading to heart disease.
High Cholesterol: Excess levels of low-density lipoprotein (LDL) cholesterol can lead to plaque formation in arteries, increasing the risk of heart attacks and strokes.
Smoking: Smoking poses a serious threat because it narrows the blood vessels, increases blood pressure and decreases the oxygen in the blood.
Diabetes: Increases the risk of heart disease as high blood sugar can damage blood vessels and the nerves that control the heart.
Obesity: Excess weight often leads to additional risk factors, like high blood pressure, high cholesterol and diabetes.
Physical Inactivity: Lack of exercise leads to obesity and increases risk factors such as high blood pressure and cholesterol.
Unhealthy Diet: A high consumption of saturated fats, trans fats, sodium, and sugar will increase the risk of CVD.
Excessive Alcohol Consumption: Over-intake of alcohol will raise your blood pressure and provide you with more calories, which can lead to weight gain.
Genetics and Family History: A family history of heart disease can increase risk, implying an underlying genetic predisposition.
Age: As the blood vessels stiffen, and the plaque thickens, the older you get, the greater the risk.
Gender: Men have an increased risk of heart attack, and post-menopausal women have a higher risk than pre-menopausal women.
Stress: Chronic stress contributes to heart disease in a variety of ways including unhealthy coping behaviors such as eating too much or smoking.
Sleep Apnea: Left untreated, sleep apnea leads to high blood pressure and other CVD risk factors.
Can cardiovascular disease be cured?
CVD is not "curable" in the conventional sense, but it can be averted to prolong life and minimize the possibility of complications. Management involves a mix of lifestyle modification, medication and even surgery or medical intervention. Important steps to combat cardiovascular disease include:
Lifestyle Changes: It's important to live a healthy life. This involves a well-balanced diet with a reduced amount of saturated fat, trans fat, cholesterol, salt, and sugar. Regular exercise, a healthy weight, a quit smoking habit and drinking moderately are steps that should be taken.
Medications: Various medications can help manage cardiovascular disease by controlling risk factors like high blood pressure, high cholesterol, and diabetes. These medications can help prevent the progression of the disease and reduce the risk of heart attacks and strokes.
Medical Procedures/Surgery: Sometimes, angioplasty, stent or bypass surgery may be required to repair and optimize the flow of blood to the heart.
Regular Monitoring and Medical Care: It's imperative to regularly visit doctors and hospitalize to keep a check on your heart health and treat any conditions that could be the cause of cardiovascular disease.
With careful compliance with a doctor's advice and lifestyle changes, most heart disease patients are able to live long and healthy lives.
IVD biomarkers for cardiovascular disease
In vitro diagnostic (IVD) tests for cardiovascular disease (CVD) often rely on a variety of biomarkers to help diagnose conditions, stratify risk, and guide treatment. Some common biomarkers used in these tests include:
Troponins (cTnI, cTnT): These proteins are released when the heart muscle injure and play an essential role in diagnosing myocardial infarction (heart attack).
B-type Natriuretic Peptide (BNP) and N-terminal proBNP (NT-proBNP): Markers of heart failure; elevated levels indicate heart stress or damage.
C-reactive Protein (CRP): An inflammatory marker, which can be linked to atherosclerosis and increased cardiovascular risk.
Lipoproteins (LDL, HDL, Total Cholesterol): Lipoprotein concentrations and ratios are used to evaluate risk for atherosclerosis and coronary artery disease.
High-sensitivity C-reactive Protein (hs-CRP): A more sensitive form of CRP used to detect chronic inflammation and predict cardiovascular events.
Lipoprotein(a): An LDL-like particle that can increase risk of CVD when present in elevated levels.
Homocysteine: High levels can contribute to arterial damage and blood clots, making it a risk factor for cardiovascular disease.
Glucose and HbA1c: Elevated blood sugar and long-term glucose levels (HbA1c) can indicate diabetes, a major risk factor for CVD.
Fibrinogen: A protein involved in blood clotting; elevated levels can increase the risk of thrombosis.
Apolipoproteins (ApoA1, ApoB): Useful in providing insights into lipid metabolism and cardiovascular risk.
Myeloperoxidase (MPO): This enzyme is associated with inflammation and oxidative stress, and elevated levels may predict cardiac events.
Copeptin: A peptide derived from the same precursor as vasopressin. Its level increases during acute myocardial infarction.
Depending on the specific cardiovascular condition being assessed, these biomarkers are used in various combinations in IVD tests.
Case Study
Case 1: He Y, Pavanello C, Hutchins PM, et al. Flipped C-Terminal Ends of APOA1 Promote ABCA1-Dependent Cholesterol Efflux by Small HDLs. Circulation. 2024 Mar 5;149(10):774-787. doi: 10.1161/CIRCULATIONAHA.123.065959. Epub 2023 Nov 29. PMID: 38018436; PMCID: PMC10913861.
The authors used model system studies of reconstituted HDL and plasma from control and lecithin-cholesterol acyltransferase (LCAT)-deficient subjects to investigate the relationships among the sizes of HDL particles, the structure of APOA1 (apolipoprotein A1) in the different particles, and the CECs of plasma and isolated HDLs.
 Fig3. Figure 2. Contact maps (A–D) of the intermolecular (Inter) and intramolecular (Intra) APOA1 (apolipoprotein A1) cross-links detected by tandem mass spectrometry (MS/MS) in different sizes of r-HDL. A, r-HDL-120. B, r-HDL-100. C, r-HDL-90. D, r-HDL-80. Red regions and green regions indicate the allowable distance of intermolecular and intramolecular peptide contacts (15.1 Å), respectively, in a molecular dynamics simulation of the LL5/5 double-belt model of APOA1. Cross-links (o) between APOA1 residues are labeled. Semiquantitative estimates of the strengths of interactions between residues were based on ion currents, and they are indicated by the colors of the circles (green, strong; yellow, medium; and red, weak).
Fig3. Figure 2. Contact maps (A–D) of the intermolecular (Inter) and intramolecular (Intra) APOA1 (apolipoprotein A1) cross-links detected by tandem mass spectrometry (MS/MS) in different sizes of r-HDL. A, r-HDL-120. B, r-HDL-100. C, r-HDL-90. D, r-HDL-80. Red regions and green regions indicate the allowable distance of intermolecular and intramolecular peptide contacts (15.1 Å), respectively, in a molecular dynamics simulation of the LL5/5 double-belt model of APOA1. Cross-links (o) between APOA1 residues are labeled. Semiquantitative estimates of the strengths of interactions between residues were based on ion currents, and they are indicated by the colors of the circles (green, strong; yellow, medium; and red, weak).Case 2: Diaz N, Perez C, Escribano AM, et al. Discovery of potent small-molecule inhibitors of lipoprotein(a) formation. Nature. 2024 May;629(8013):945-950. doi: 10.1038/s41586-024-07387-z. Epub 2024 May 8. PMID: 38720069; PMCID: PMC11111404.
The researchers show that the first step of Lp(a) formation can be inhibited through small-molecule interactions with apo(a) KIV7-8. They identify compounds that bind to apo(a) KIV7-8, and, through chemical optimization and further application of multivalency, and they create compounds with subnanomolar potency that inhibit the formation of Lp(a).
 Fig4. Multivalency increases the potency and efficacy of Lp(a) reduction. a, Percentage change in the steady-state levels of Lp(a) in LPA × ApoB100 transgenic mice after five days of BID oral dosing with LSN3441732. Data are from one experiment with n = 5 per group, shown as mean ± s.e.m. with individuals plotted as circles. Two-sided P values were calculated using one-way ANOVA with Dunnett's comparison to vehicle. b, Percentage change from baseline in the steady-state levels of Lp(a) in female cynomolgus monkeys during 14 days of BID oral dosing (n = 8 per group except n = 9 for the vehicle group) with LSN3441732 in a single experiment. Box plots as in Fig. 1f. Two-sided P values are from a repeated measures ANOVA with Bonferroni comparisons to vehicle at each time point. The null hypothesis was rejected at P < 0.05.
Fig4. Multivalency increases the potency and efficacy of Lp(a) reduction. a, Percentage change in the steady-state levels of Lp(a) in LPA × ApoB100 transgenic mice after five days of BID oral dosing with LSN3441732. Data are from one experiment with n = 5 per group, shown as mean ± s.e.m. with individuals plotted as circles. Two-sided P values were calculated using one-way ANOVA with Dunnett's comparison to vehicle. b, Percentage change from baseline in the steady-state levels of Lp(a) in female cynomolgus monkeys during 14 days of BID oral dosing (n = 8 per group except n = 9 for the vehicle group) with LSN3441732 in a single experiment. Box plots as in Fig. 1f. Two-sided P values are from a repeated measures ANOVA with Bonferroni comparisons to vehicle at each time point. The null hypothesis was rejected at P < 0.05.
