Cardiovascular Biology
Creative BioMart Cardiovascular Biology Product List
Immunology Background
Background
Cardiovascular biology is the study of the mechanisms of cardiovascular physiology and pathophysiology. To be specific, cardiovascular biology encompasses the study of the heart, blood vessels, and the regulatory mechanisms that govern the circulation of blood throughout the body. In the field of cardiovascular biology, some popular topics include Angiogenesis, Coagulation, Early Mesodermal Lineage Markers, Hemangioblast Markers, Lipid/Cholesterol Metabolism, Vascular Endothelium, and Vascular Smooth Muscle. Cardiovascular disease is crucial not only for understanding how the cardiovascular system functions under normal conditions but also for unraveling the co mplexities of cardiovascular diseases and developing effective therapies.
Cardiovascular System
The cardiovascular system, also known as the circulatory system, is vital for sustaining life. It is responsible for the delivery of oxygen and nutrients to tissues and the removal of carbon dioxide and metabolic wastes. This system includes the heart, blood vessels, and blood. The study of cardiovascular biology dates back to ancient civilizations, but significant advancements were made in the 17th century when William Harvey described the systemic circulation and the properties of blood being pumped by the heart. Since then, cardiovascular biology has evolved into a sophisticated field integrating aspects of molecular biology, physiology, genetics, and pharmacology.
Heart
The heart is a muscular organ roughly the size of a fist, located in the thoracic cavity. It consists of four chambers: two atria and two ventricles. The right side of the heart receives deoxygenated blood from the body and pumps it to the lungs for oxygenation (pulmonary circulation), while the left side receives oxygenated blood from the lungs and pumps it to the rest of the body (systemic circulation). The heart's pumping action is regulated by a conduction system that includes the sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, and Purkinje fibers.
Blood Vessels
Blood vessels are classified into arteries, veins, and capillaries. Arteries carry oxygen-rich blood away from the heart to the tissues, while veins return oxygen-depleted blood back to the heart. Capillaries are tiny vessels where the exchange of gases, nutrients, and waste products occurs. The structure of blood vessels is adapted to their function; for example, arteries have thick elastic walls to withstand high pressure, while veins have valves to prevent backflow of blood.
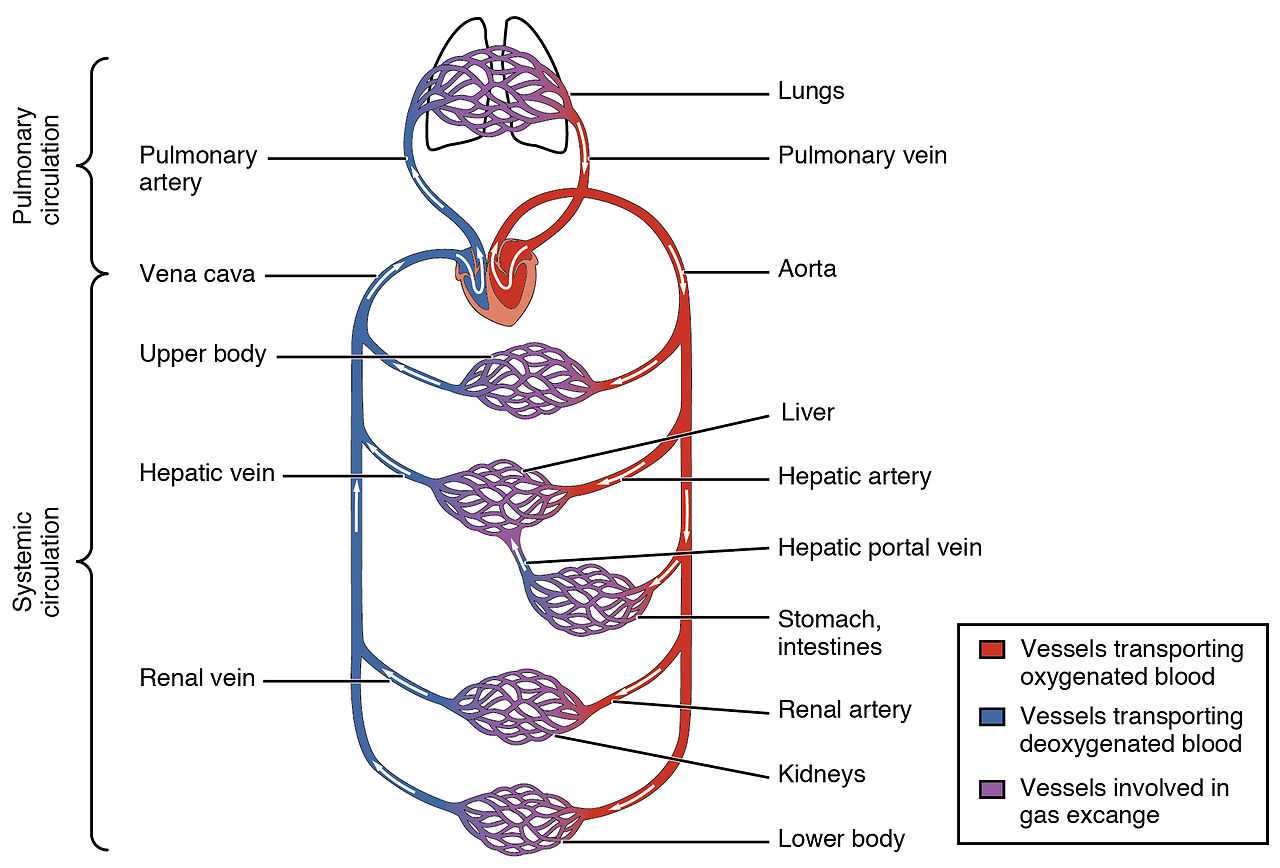 Fig. 1: The human circulatory system (simplified).
Fig. 1: The human circulatory system (simplified).Cardiovascular Regulation
The cardiovascular system is tightly regulated to maintain homeostasis. Key regulatory mechanisms include neural control, hormonal control, and local control.
Neural Control
The autonomic nervous system (ANS) plays a crucial role in cardiovascular regulation. The sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS) exert opposing effects. The SNS increases heart rate and contractility and constricts blood vessels, thereby increasing blood pressure. In contrast, the PNS decreases heart rate and promotes vasodilation, reducing blood pressure. These responses are mediated by neurotransmitters such as norepinephrine and acetylcholine.
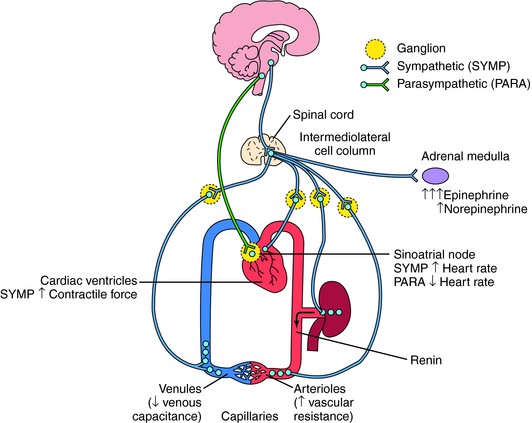 Fig. 2: Effects of the autonomic nervous system on blood pressure control. Vascular resistance is affected almost exclusively by the sympathetic nervous system, whereas cardiac output is regulated by both sympathetic and parasympathetic influences.
Fig. 2: Effects of the autonomic nervous system on blood pressure control. Vascular resistance is affected almost exclusively by the sympathetic nervous system, whereas cardiac output is regulated by both sympathetic and parasympathetic influences.Hormonal Control
Several hormones are involved in the regulation of the cardiovascular system. For instance, adrenaline and noradrenaline from the adrenal medulla enhance the SNS effects. The renin-angiotensin-aldosterone system (RAAS) regulates blood volume and systemic vascular resistance. It regulates your blood pressure by increasing sodium (salt) reabsorption, water reabsorption (retention) and vascular tone (the degree to which your blood vessels constrict, or narrow). The RAAS begins with the release of renin, an enzyme produced by the kidneys in response to low blood pressure, low sodium levels, or sympathetic nervous system stimulation. Renin converts then angiotensinogen, a protein produced by the liver, into angiotensin I. Angiotensin I is converted into angiotensin II by the angiotensin-converting enzyme (ACE), primarily in the lungs. Angiotensin II constricts blood vessels, increasing systemic vascular resistance and raising blood pressure; stimulates the adrenal cortex to release aldosterone; and stimulates release of antidiuretic Hormone (ADH). Both Aldosterone and ADH promote water reabsorption. This reabsorption increases blood volume, contributing to higher blood pressure. Through vasoconstriction and increased blood volume, the RAAS ensures adequate blood pressure and perfusion to vital organs. It maintains homeostasis by adjusting blood pressure and fluid balance in response to physiological changes.
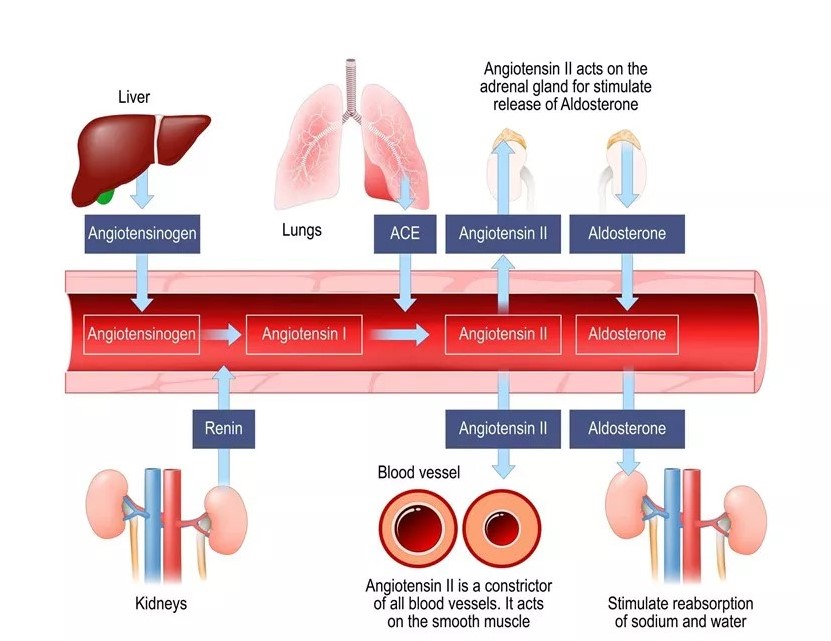 Fig. 3: Classical Renin-Angiotensin-Aldosterone System.
Fig. 3: Classical Renin-Angiotensin-Aldosterone System.Local Control
Local factors also regulate blood flow within tissues. Endothelial cells lining the blood vessels release substances such as nitric oxide (NO), which induces vasodilation, and endothelin, which causes vasoconstriction. These local mechanisms ensure adequate tissue perfusion according to metabolic needs.
Cardiovascular Diseases
Cardiovascular diseases (CVDs) are a leading cause of morbidity and mortality worldwide, taking an estimated 17.9 million lives each year. They encompass a range of conditions affecting the heart and blood vessels, including coronary artery disease (CAD), hypertension, heart failure, and stroke.
Coronary Artery Disease (CAD)
CAD is characterized by the narrowing or blockage of coronary arteries due to atherosclerosis, the buildup of plaques composed of fat, cholesterol, and other substances. This reduces blood flow to the heart muscle, leading to angina (chest pain) or myocardial infarction (heart attack).
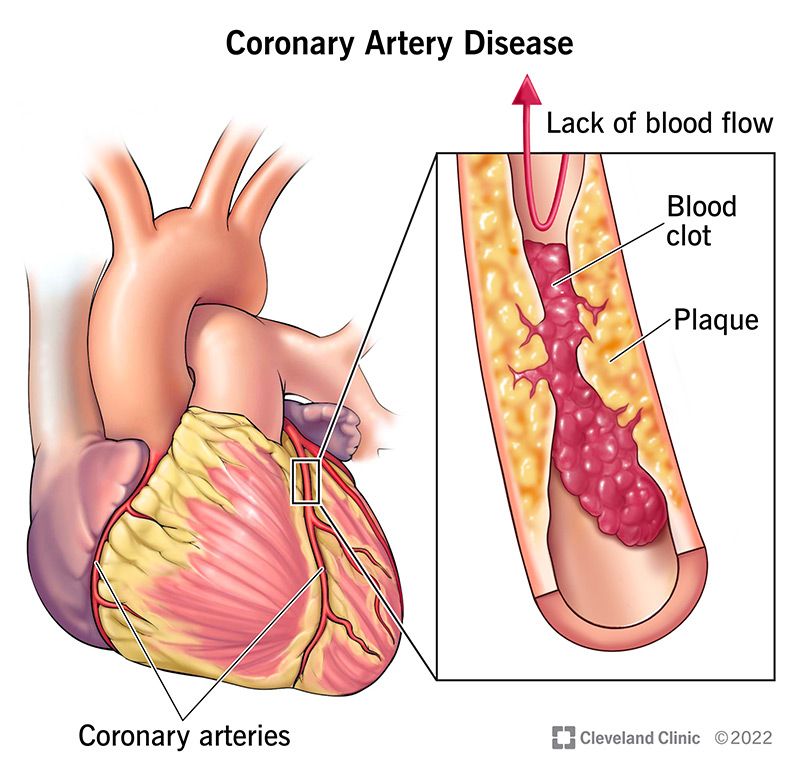 Fig. 4: The cause of CAD is the accumulation of plaque in the arteries that supply blood to heart, leading to the formation of blood clots.
Fig. 4: The cause of CAD is the accumulation of plaque in the arteries that supply blood to heart, leading to the formation of blood clots.Cerebrovascular Disease
Cerebrovascular disease refers to a group of conditions that affect the blood vessels and blood supply to the brain. These conditions can lead to a range of problems, including stroke, transient ischemic attack (TIA), aneurysms, and vascular malformations. Cerebrovascular diseases are a major cause of disability and death worldwide.
Stroke
A stroke occurs when the blood supply to part of the brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. This can be due to a blocked artery (ischemic stroke) or a ruptured blood vessel (hemorrhagic stroke). Prompt treatment is crucial to minimize brain damage and improve outcomes.
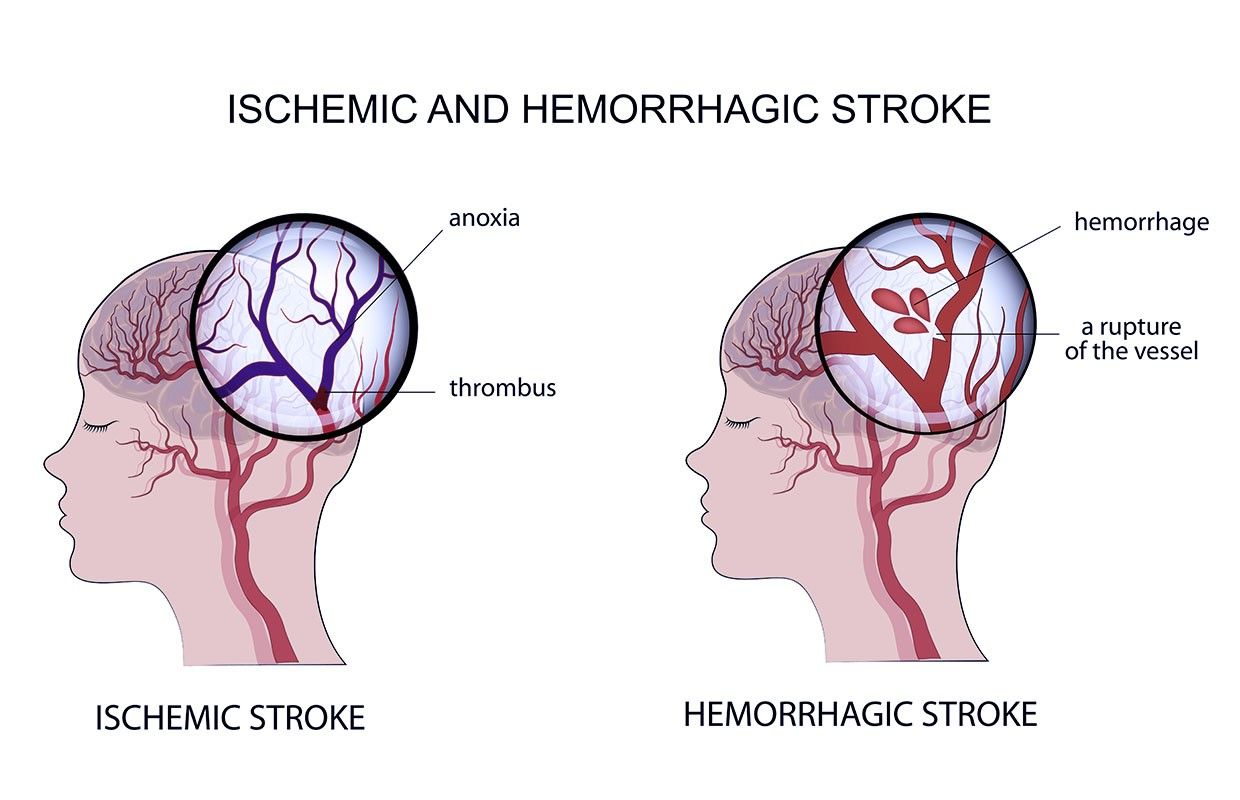 Fig. 5: Types of strokes: ischemic stroke and hemorrhagic stroke.
Fig. 5: Types of strokes: ischemic stroke and hemorrhagic stroke.Transient Ischemic Attack (TIA)
A TIA, often called a mini-stroke, is a temporary period of symptoms similar to those of a stroke. A TIA is caused by a temporary decrease in blood supply to part of the brain and typically lasts a few minutes to a few hours, without causing permanent damage. However, a TIA is a warning sign of a potential future stroke and requires medical attention.
Aneurysms
A cerebral aneurysm is a weak or thin spot on a blood vessel in the brain that balloons out and fills with blood. A ruptured aneurysm can cause a hemorrhagic stroke, leading to serious complications or death. According to the shape, aneurysm is divided into three types: fusiform-shaped aneurysm (Bulges or balloons out on all sides of the aorta; relatively more common); saccular-shaped aneurysm (Bulges or balloons out only on one side); and pseudoaneurysm or false aneurysm) (Enlargement of only the outer layer of the blood vessel wall).
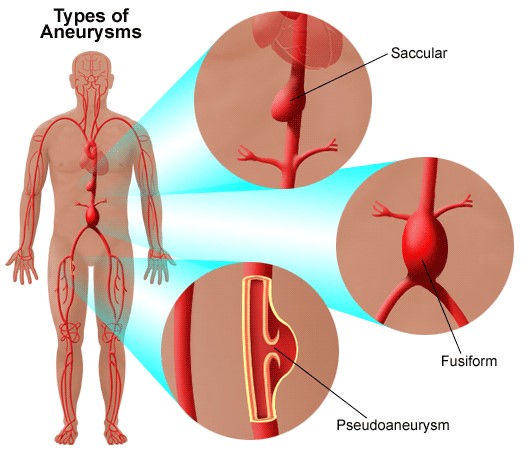 Fig. 6: The three different types of aneurysms: Fusiform, saccular, and pseudoaneurysm.
Fig. 6: The three different types of aneurysms: Fusiform, saccular, and pseudoaneurysm.Vascular Malformations
These are abnormal connections between blood vessels in the brain, including arteriovenous malformations (AVMs) and cavernous malformations. These malformations can disrupt normal blood flow and increase the risk of bleeding in the brain.
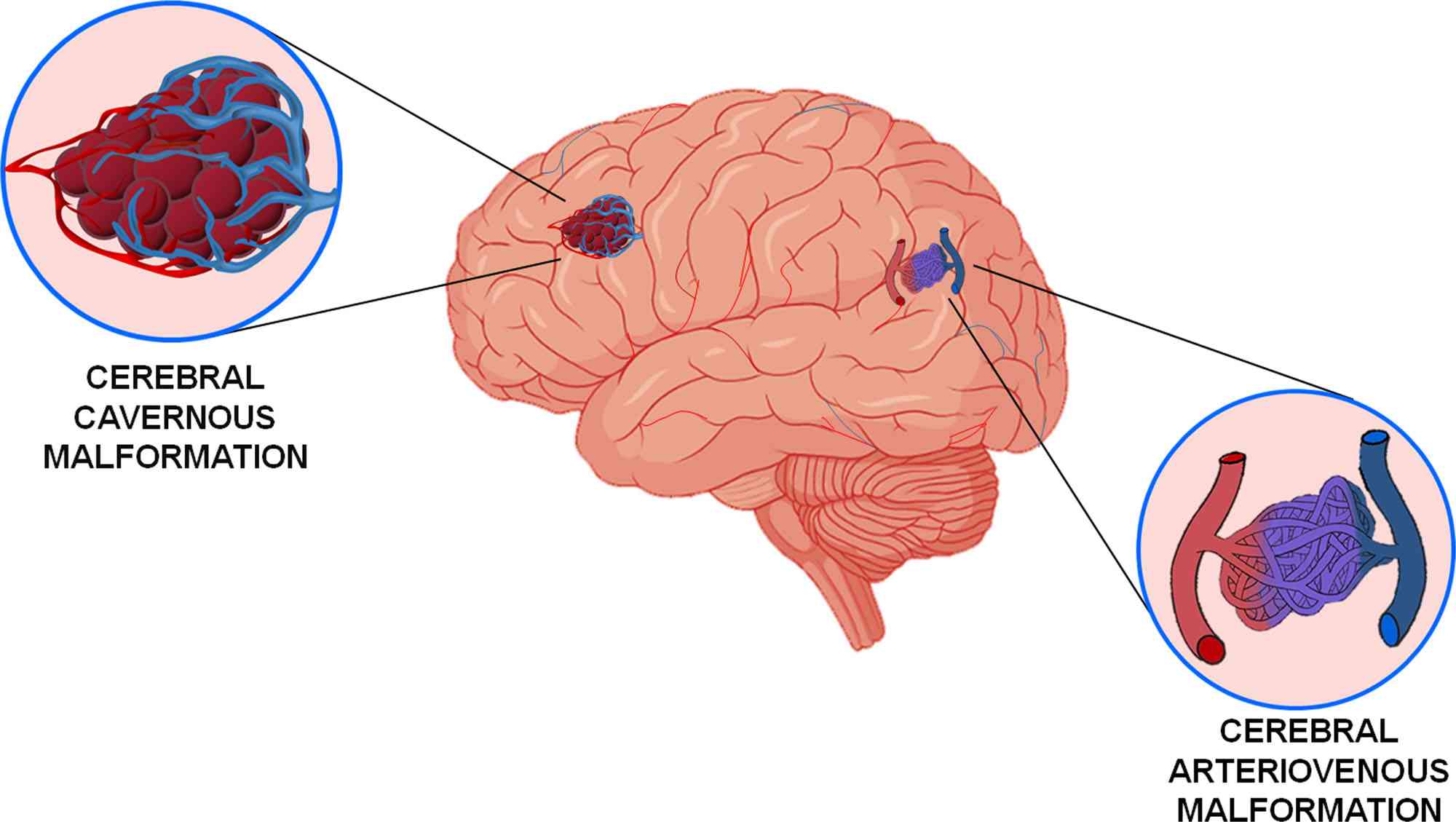 Fig. 7: Vascular malformations of the brain. Arteriovenous and cerebral cavernous malformations comprise the major vascular malformations of the brain.
Fig. 7: Vascular malformations of the brain. Arteriovenous and cerebral cavernous malformations comprise the major vascular malformations of the brain.Rheumatic Heart Disease
Rheumatic heart disease starts as a sore throat from a bacterium called Streptococcus pyogenes (group A Streptococcus) which can pass easily from person to person in the same way as other upper respiratory tract infections. Strep infections are most common in childhood.
In some people, repeated strep infections cause the immune system to react against the tissues of the body including inflaming and scarring the heart valves. This is what is referred to as rheumatic fever. Rheumatic heart disease results then from the inflammation and scarring of heart valves caused by rheumatic fever.
Hypertension
Hypertension, or high blood pressure, is a condition where the force of the blood against the artery walls is consistently too high. It is a major risk factor for other CVDs, including stroke and heart failure. Causes of hypertension can be multifactorial, involving genetic predisposition, lifestyle factors, and underlying health conditions.
Heart Failure
Heart failure occurs when the heart is unable to pump blood effectively to meet the body's needs. It can result from conditions such as CAD, hypertension, or cardiomyopathy. Symptoms include shortness of breath, fatigue, and fluid retention.
Therapy of Cardiovascular Diseases
Advances in medical research have led to various therapeutic approaches for managing cardiovascular diseases. These include lifestyle modifications, pharmacological treatments, surgical interventions, and emerging therapies.
Lifestyle Modifications
Lifestyle changes are foundational in managing and preventing CVDs. These include adopting a healthy diet rich in fruits, vegetables, and whole grains; engaging in regular physical activity; avoiding tobacco use; and managing stress. Weight management and moderating alcohol intake are also important.
Pharmacological Treatments
Medications play a vital role in treating cardiovascular diseases.
- Antihypertensive drugs can be classified into four main groups according to their mechanism of action: those that act in the renin angiotensin aldosterone system (RAAS), either by inhibiting angiotensin converting enzyme (ACE), blocking the angiotensin type 1 receptor (AT1R), directly inhibiting renin action, or by antagonizing aldosterone binding to its receptor; those that act blocking the calcium channels, which can block either dihydropyridine or non-dihydropyridine calcium channels; beta blockers that block the β-adrenergic receptors; and diuretics, which decrease the volume in the circulatory system.
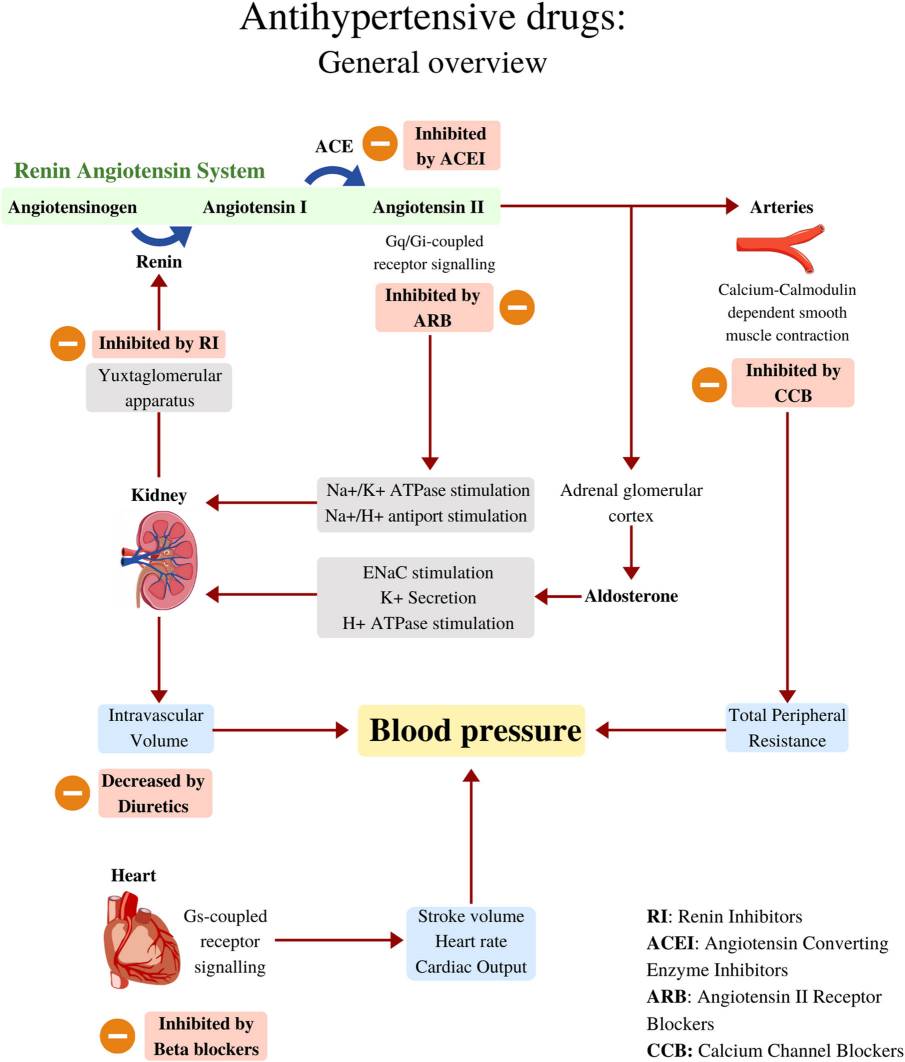 Fig. 8: Antihypertensive drugs: General overview.
Fig. 8: Antihypertensive drugs: General overview.- Statins are commonly prescribed to lower cholesterol levels and reduce the risk of CAD. Their mode of action is primarily via inhibition of HMG-CoA (hydroxymethylglutaryl-coenzyme A) reductase, the rate-limiting enzyme in the cholesterol biosynthesis pathway.
- Antiplatelet agents like aspirin and anticoagulants prevent blood clots, reducing the risk of heart attacks and strokes. The mechanisms of action of most commonly used antiplatelet therapies are illustrated in the Figure. Aspirin (acetylsalicylic acid, ASA) is the most widely used antiplatelet agent and irreversibly inhibits the enzyme cyclooxygenase-1 (COX-1) in platelets, reducing production of thromboxane A2 (TXA2).
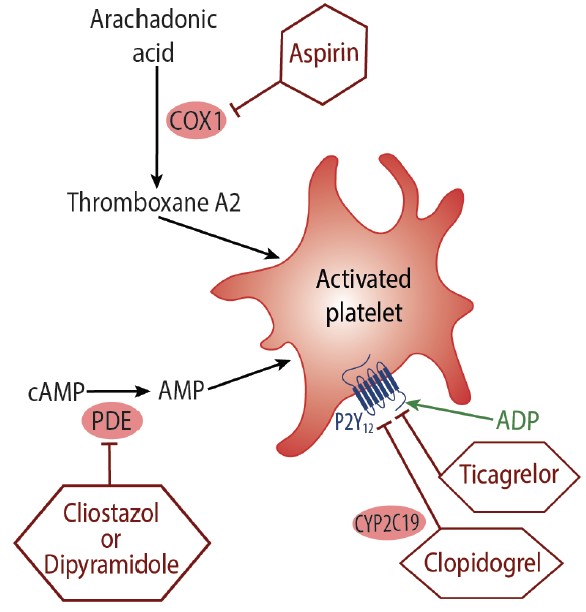 Fig. 9: Mechanism of action for antiplatelet medications. (green arrow signifies stimulation, red arrow inhibition). Abbreviations: ADP, adenosine diphosphate; AMP, adenosine monophosphate; cAMP, cyclic adenosine monophosphate; COX-1, cyclooxygenase 1.
Fig. 9: Mechanism of action for antiplatelet medications. (green arrow signifies stimulation, red arrow inhibition). Abbreviations: ADP, adenosine diphosphate; AMP, adenosine monophosphate; cAMP, cyclic adenosine monophosphate; COX-1, cyclooxygenase 1.Surgical Interventions
In cases where medications and lifestyle changes are insufficient, surgical interventions may be necessary. Coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) are common procedures for treating severe CAD. Heart valve repair or replacement surgery is performed for valve disorders. In advanced heart failure, heart transplantation or the implantation of a ventricular assist device (VAD) may be required.
Emerging Therapies
Emerging therapies hold promise for more effective treatment of CVDs. These include gene therapy, which aims to correct genetic defects causing heart disease, and stem cell therapy, which seeks to regenerate damaged heart tissue. Additionally, advances in medical technology, such as minimally invasive surgical techniques and innovative medical devices, are enhancing patient outcomes.
Cardiovascular biology is a dynamic and multifaceted field essential for understanding the mechanisms of the cardiovascular system, the pathophysiology of cardiovascular diseases, and the development of innovative therapies. As research continues to unravel the complexities of the cardiovascular system, there is hope for more effective prevention, diagnosis, and treatment of cardiovascular diseases, ultimately improving the quality of life for millions of people worldwide.
Case Study
Case 1: Ferrario, CM.; et al. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005 May 24;111(20):2605-10.
Angiotensin-converting enzyme 2 (ACE2) has been identified as a novel regulator of cardiac function and arterial pressure by converting angiotensin II (Ang II) into angiotensin-(1–7) [Ang-(1–7)], a heptapeptide known for its vasodilatory and antitrophic properties. Given that ACE2 is the only recognized human homolog of ACE and is insensitive to blockade by ACE inhibitors, researchers aimed to investigate the impact of ACE inhibition on the expression of the ACE2 gene.
Blood pressure, cardiac rate, and plasma and cardiac tissue levels of Ang II and Ang-(1–7), together with cardiac ACE2, neprilysin, Ang II type 1 receptor (AT1), and mas receptor mRNAs, were measured in Lewis rats 12 days after continuous administration of vehicle, lisinopril, losartan, or both drugs combined in their drinking water. The results indicate that selective blockade of either Ang II synthesis or activity induced increases in cardiac ACE2 gene expression and cardiac ACE2 activity, whereas the combination of losartan and lisinopril was associated with elevated cardiac ACE2 activity but not cardiac ACE2 mRNA. Although the predominant effect of ACE inhibition may result from the combined effect of reduced Ang II formation and Ang-(1–7) metabolism, the antihypertensive action of AT1 antagonists may in part be due to increased Ang II metabolism by ACE2.
The effects of lisinopril and losartan alone or in combination on cardiac ACE2 activity were compared. Rats medicated with losartan or the combination of losartan and lisinopril showed significant increases in ACE2 activity, whereas ACE2 activity did not change in the lisinopril-treated group.
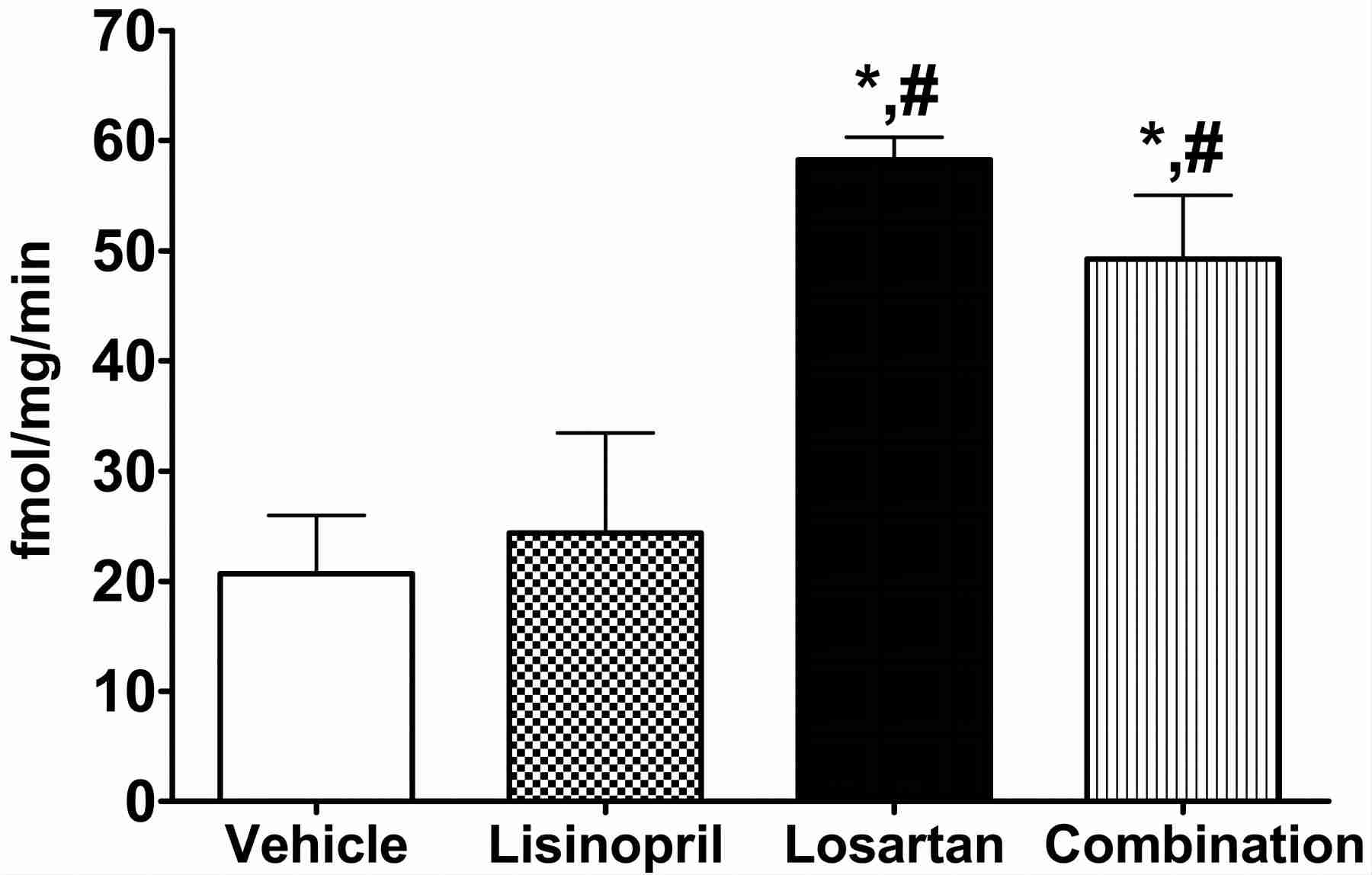 Fig. 10: Effects of various treatments on ACE2 activity in Lewis rats. Values are mean±SEM. *P<0.05 vs vehicle; #P<0.05 versus lisinopril.
Fig. 10: Effects of various treatments on ACE2 activity in Lewis rats. Values are mean±SEM. *P<0.05 vs vehicle; #P<0.05 versus lisinopril.Case 2: Praticò, D.; et al. Acceleration of atherogenesis by cox-1-dependent prostanoid formation in low density lipoprotein receptor knockout mice. Proceedings of the National Academy of Sciences, vol. 98, no. 6, Mar. 2001, pp. 3358–63.
Prostacyclin (PGI2), product of cyclooxygenase (COX), inhibits platelet activation and vascular smooth-muscle cell migration and proliferation. Biochemically selective inhibition of COX-2 reduces PGI2 biosynthesis substantially in humans. Because deletion of the PGI2 receptor accelerates atherogenesis in the fat-fed low density lipoprotein receptor knockout mouse, Praticò et al. wished to determine whether selective inhibition of COX-2 would accelerate atherogenesis in this model. To address this hypothesis, researcher used dosing with nimesulide, which inhibited COX-2 ex vivo, depressed urinary 2,3 dinor 6-keto PGF1α by approximately 60% but had no effect on thromboxane formation by platelets, which only express COX-1. By contrast, the isoform nonspecific inhibitor, indomethacin, suppressed platelet function and thromboxane formation ex vivo and in vivo, coincident with effects on PGI2 biosynthesis indistinguishable from nimesulide. Indomethacin reduced the extent of atherosclerosis by 55±4%, whereas nimesulide failed to increase the rate of atherogenesis.
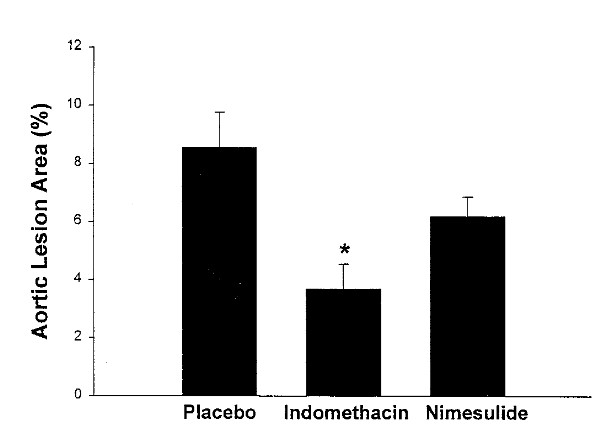 Fig. 11: Percentage of total aortic-lesion areas in LDLR-KO mice (26 weeks of age) on Western-type diet receiving placebo, indomethacin, or nimesulide for 18 weeks (*, P < 0.001 vs. placebo).
Fig. 11: Percentage of total aortic-lesion areas in LDLR-KO mice (26 weeks of age) on Western-type diet receiving placebo, indomethacin, or nimesulide for 18 weeks (*, P < 0.001 vs. placebo).References
- Carlos-Escalante, José A., et al. "The Use of Antihypertensive Drugs as Coadjuvant Therapy in Cancer." Frontiers in Oncology, vol. 11, May 2021.
- Ferrario, Carlos M., et al. "Effect of Angiotensin-Converting Enzyme Inhibition and Angiotensin II Receptor Blockers on Cardiac Angiotensin-Converting Enzyme 2." Circulation, vol. 111, no. 20, May 2005, pp. 2605–10.
- Indraswari, et al, "Antiplatelet Therapies After Ischemic Stroke." Practical Neurology, accessed 16 July 2024.
- Praticò, Domenico, et al. "Acceleration of Atherogenesis by COX-1-Dependent Prostanoid Formation in Low Density Lipoprotein Receptor Knockout Mice." Proceedings of the National Academy of Sciences, vol. 98, no. 6, Mar. 2001, pp. 3358–63.
- Venugopal, Vani, and S. Sumi. "Molecular Biomarkers and Drug Targets in Brain Arteriovenous and Cavernous Malformations: Where Are We?" Stroke, vol. 53, no. 1, Jan. 2022, pp. 279–89.

