Uncategorized Friday, 2024/07/19
Type I interferon (IFN-I) and IFN - γ can promote anti-tumor immunity by enhancing the body's T-cell response. Paradoxically, IFN - γ can promote T cell depletion by activating immune checkpoints. The downstream regulatory mechanisms of these different responses are currently unclear to researchers. Recently, a research report titled "Opposing tumor-cell-intrinsic and -extrinsic roles of the IRF1 transcription factor in antitumor immunity" was published in the journal Cell Reports. Scientists from the David Geffen School of Medicine at the University of California, and other institutions have uncovered the role and detailed information of a special protein called interferon regulatory factor (IRF1) in cancer progression and therapy response, which is expected to provide new insights into improving the efficacy of cancer immunotherapy.
In the article, researchers revealed how IRF1 hinders and helps the body's immune response to resist tumors, depending on which cells the IRF1 protein is found in. Professor Philip Scumpia said, 'We all know that IRF1 plays a crucial role in regulating the body's anti-tumor immunity. However, there are still conflicting reports on whether IRF1 promotes or inhibits the body's anti-tumor immunity. What surprises us is that the role of IRF1 depends on the cells that express it, which may explain these conflicting reports. Our research has added complexity to understanding IRF1 and its role in immunotherapy.'
Our Related Proteins
Nowadays, immunotherapy remains a powerful tool in cancer treatment, as it can recognize and attack cancer cells by utilizing the body's immune system. Although immunotherapy can successfully treat certain types of cancer and provide long-term disease remission for some patients, it is still not effective for all patients. Understanding the mechanisms by which proteins such as IRF1 function may help to effectively improve human immunotherapy strategies and make them more effective for a wider range of patients; To elucidate the crucial role of IRF1 in tumor growth and immune response, researchers observed what happens when IRF1 is absent in tumor cells and surrounding cells.
Researcher Prabhat Purbey said that our previous research found that cells exposed to ionizing radiation (a
well-known cancer therapy) can induce an immune response in the body through IRF1, so we wanted to observe whether
IRF1 can also regulate similar immune responses in growing tumors. Firstly, researchers developed IRF1-deficient
clones of various tumor cells and compared the growth of these genetically modified tumors with that of normal
tumors. Then, histological methods and flow cytometry were used to evaluate the infiltration of immune cells.
Subsequently, researchers analyzed the effects of immune checkpoint blockade therapy (a type of immunotherapy) on
these tumors and performed single-cell RNA sequencing to understand the activation status of immune cells.
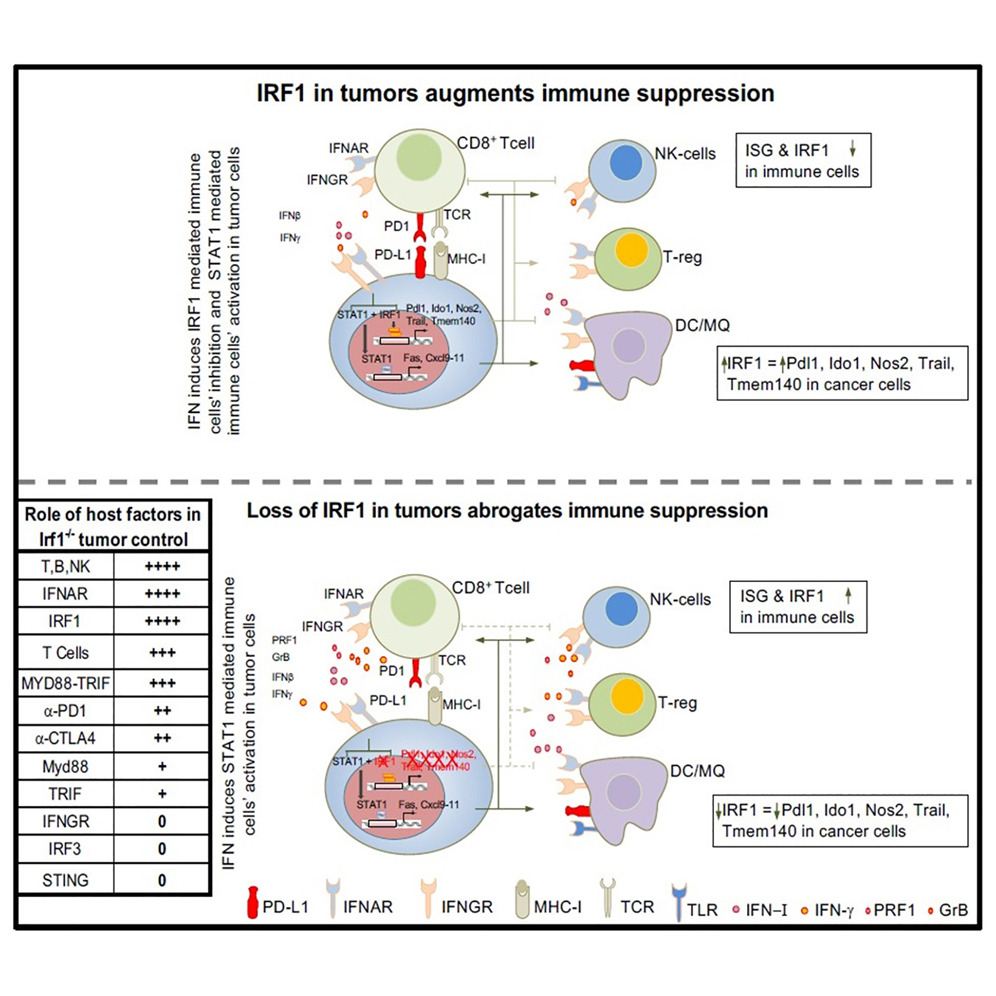 Researchers have found that the presence of IRF1 in tumor cells can weaken the host's immune response by promoting T
cell depletion and affecting toll-like receptors and type I interferon response. This occurs because IRF1 in tumor
cells can increase the levels of various immune checkpoints, including IDO-1
and PD-L1, which can inhibit T-cell activity and alter the expression of
proteins involved in antigen presentation. However, IRF1 is crucial for the development and recruitment of immune
cells, as well as the function of cytotoxic T cells and natural killer cells, which are key immune cells capable of
directly attacking tumor cells. Researcher Scumpia said that these findings suggest that reducing the level of IRF1
in tumor cells or activating it in immune cells can enhance the efficacy of cancer therapy by enhancing the body's
natural anti-tumor immunity. Now we have a clearer understanding of where IRF1 can affect the efficacy of
immunotherapy and how to adjust it to help resist cancer.
Researchers have found that the presence of IRF1 in tumor cells can weaken the host's immune response by promoting T
cell depletion and affecting toll-like receptors and type I interferon response. This occurs because IRF1 in tumor
cells can increase the levels of various immune checkpoints, including IDO-1
and PD-L1, which can inhibit T-cell activity and alter the expression of
proteins involved in antigen presentation. However, IRF1 is crucial for the development and recruitment of immune
cells, as well as the function of cytotoxic T cells and natural killer cells, which are key immune cells capable of
directly attacking tumor cells. Researcher Scumpia said that these findings suggest that reducing the level of IRF1
in tumor cells or activating it in immune cells can enhance the efficacy of cancer therapy by enhancing the body's
natural anti-tumor immunity. Now we have a clearer understanding of where IRF1 can affect the efficacy of
immunotherapy and how to adjust it to help resist cancer.
Although further research is needed to clarify whether targeting IRF1 in tumor cells or immune cells can produce benefits after tumor growth, this study may help elucidate why IRF1 has been shown to be a barrier or aid in different cancer situations. By manipulating the potential of IRF1 in a specific way or changing the way we approach cancer immunotherapy, researchers aim to translate these findings into novel therapies that bring hope to cancer patients and improve their treatment outcomes.
In summary, in this study, researchers found that the expression of IRF1 in tumor cells inhibits the host body's IFN-I and IRF1-dependent anti-tumor immunity, thereby promoting the immune escape of cancer cells and tumor growth.
Related Products and Services
Targets of CAR-T Cell Therapy Cytokines Cancer Drug Targets Immune Checkpoint Proteins Protein Engineering Services Protein Interaction Service Protein Expression and Purification Services Drug Discovery Screening Protein Pathway Profiling
Reference Prabhat K Purbey, Joowon Seo, Manash K Paul, et al. Opposing tumor-cell-intrinsic and -extrinsic roles of the IRF1 transcription factor in antitumor immunity, Cell Reports (2024). DOI:10.1016/j.celrep.2024.114289
