Uncategorized Friday, 2025/03/14
In a new study, researchers from Karolinska Institute and Astrid Lindgren Children's Hospital have determined how children's immune systems respond to different types of cancer based on age. This discovery reveals significant differences in immune responses between children and adults, and may provide new tailored treatment options for children with cancer.
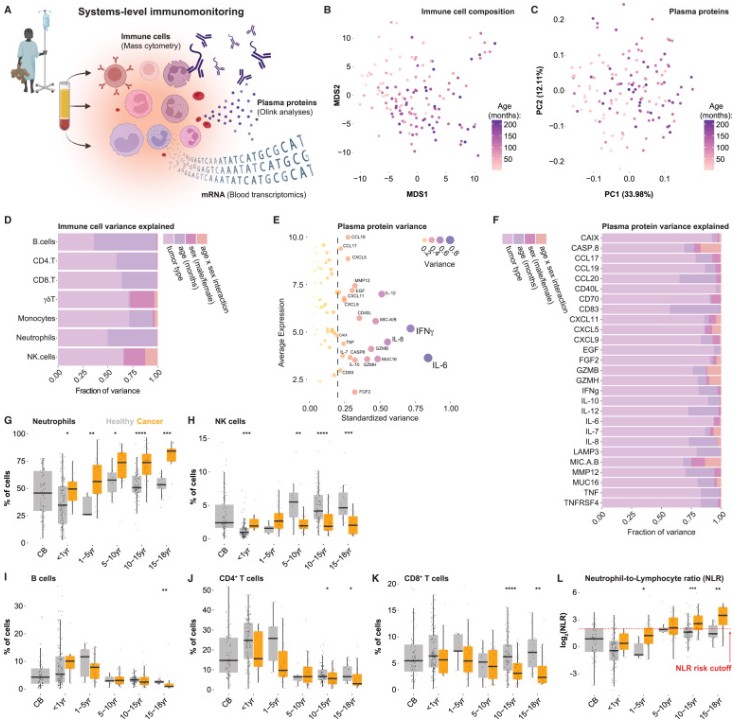
The relevant research results were published online in the Cell journal, with the paper titled “Systems-level immunomonitoring in children with solid tumors to enable precision medicine”.
“The activation of the immune system is crucial for our ability to fight cancer, but there are differences between children and adults. If we want to treat childhood cancer correctly, we need to understand how the immune system of children with cancer is activated and regulated, and what factors affect their immune response, “ said Petter Brodin, corresponding author of the paper, professor of pediatric immunology at the Department of Women and Children's Health at Karolinska Institute, and pediatrician at Astrid Lindgren Children's Hospital
New dimensions of precision medicine
This study included 191 children aged 0 to 18 who were diagnosed with different types of solid tumors at Astrid Lindgren Children's Hospital between 2018 and 2024. These authors analyzed tumor tissue and blood samples to identify gene mutations in tumors and determine which genes are active and which are inactive in the immune system.
Professor Brodin explained, “Precision medicine for cancer primarily focuses on the characteristics of tumors. By characterizing the immune system, we introduce a whole new dimension that will help shape the future of childhood cancer treatment.”
The difference between children and adults
These research results indicate that the immune systems of children and adults respond differently to cancer, and different tumors activate the immune response to varying degrees.
Professor Brodin said, “We can see that tumors in children usually have lower levels of inflammation and fewer mutations, which means they may not be as unfamiliar to the immune system, so the immune system will not attack tumors as strongly as before.”
“That being said, individual differences are significant, highlighting the importance of precision medicine, which means adjusting treatment based on individual patients. Our research shows how to achieve this in practice.”
Immunotherapy is not suitable for children
These results may explain why children cannot benefit from immunotherapy such as immune checkpoint inhibitors. Professor Brodin said, “This requires activating immune cells to fight tumors. We found that children's immune cells are often not initially activated to fight tumors, which means immune checkpoint inhibitors do not work. Children may need different types of immunotherapy that focus more on triggering immune cells to attack tumor cells from scratch.”
Tracking children's immune responses
After tracking the immune responses of some children over time and during treatment, these authors were able to measure changes in the population of cytotoxic T cells (immune cells responsible for killing tumors).
He continued, “This is something we may use in clinical practice today to assess treatment efficacy and adjust treatment for each patient. We will now test it on a larger scale because we believe it can serve as a useful supplement to tumor genetic analysis already conducted in routine care.”
Related Products and Services
PROTAC Targets
Cell and Gene Therapy
Targets of CAR-T Cell Therapy
Cancer Drug Targets
Immune Checkpoint Proteins
Protein Engineering Services
Protein Interaction Service
Protein Expression and Purification Services
Drug Discovery Screening
Protein Pathway Profiling
Reference
Systems-level immunomonitoring in children with solid tumors to enable precision medicine
Chen, Qi et al. Cell, Volume 188, Issue 5, 1425 - 1440.e11
